Post-donation guidelines
Contents
- 1 Purpose of Post-donation Guidelines and Background Information
- 2 Private GP Appointments
- 3 Emotional and Physical Recovery
- 4 Peripheral Blood Stem Cell (PBSC) and Bone Marrow (BM) Recovery Graphs
- 5 Guidance for Short Term Post-Donation Symptoms A-Z
- 5.1 Abdominal Swelling and Pain or Discomfort
- 5.2 Back Pain
- 5.3 Bruising at Donation Site
- 5.4 Headache
- 5.5 Infection at Donation Site
- 5.6 Infections (Other), and Viruses
- 5.7 Muscle Cramps
- 5.8 Nausea, Vomiting, and Diarrhoea
- 5.9 Pain and/or Tingling at the Donation Site
- 5.10 Pain at G-CSF Injection Site
- 5.11 Rash
- 5.12 Restless Legs
- 5.13 Tiredness
- 6 References
- 7 Version
Purpose of Post-donation Guidelines and Background Information
These guidelines are to aid the Donor Follow Up (DFU) team to provide consistent advice to donors, and to gather the necessary information to pass on to the Medical Team for further advice as appropriate. The DFU team is the main point of contact for Anthony Nolan, NHSBT, and Cell and Gene Therapy donors post-donation and is responsible for following up with each donor until they are fully recovered.
The advice noted in this document should not replace contacting the Medical Team if there is any concern about a donor’s recovery. If a donor is experiencing severe symptoms and is being supported by the Medical Team; the Quality Team must be informed, and if appropriate, an Internal Serious Adverse Reaction (SAR) should be raised following the process in the Donor Follow Up Procedure SOP (DOC 2386).
This version of the document is a reference for common symptoms that are mentioned:
- during the day 2/3 follow-up call
- on the day 7 health survey
- on the day 30 feedback form
These communications are managed following the process documented in the Donor Follow Up Procedure SOP (DOC 2386). Any symptoms or medical issues relating to donation that are ongoing at 30 days post-donation, should be flagged to the Medical Team for advice.
Late-occurring issues: If a donor contacts Anthony Nolan at any time after 30 days post-donation or at any point during the 10-year follow up period with a medical issue they believe is linked to their donation, this should be discussed with the Medical Team for advice, and this advice documented in the next version of these guidelines if appropriate.
If a donor informs us of developing a medical condition at any time post-donation that is not related to donation (e.g. a cancer diagnosis), this must be checked against the Anthony Nolan Medical Guidelines wiki page. This is to determine if the donor can remain on the register, if the condition may be relevant to the patient’s treatment, and if the Transplant Centre (TC) needs to be informed. The Medical Team should be contacted for advice and this guidance added to the next version of this document.
All conversations between the donor and the Medical Team, or between donor and DFU team should be documented in the notes section of the Follow-Up Record in CORAL. The process for using the Follow Up record is documented in the Donor Follow Up Procedure SOP (DOC 2386).
Private GP Appointments
If a donor is unable to access their GP, or their GP is unable to provide a timely appointment, DFU can arrange referral to a private GP practice close to the donor’s home and cover the costs. This does not need to be raised as a SAR to track the cost if it is just a one-off appointment. If a series of appointments is required, for example a course of physio sessions, it should be raised as a SAR.
Emotional and Physical Recovery
The Young Donor Project (1) found a possible link between emotional and physical recovery post-donation. Donors who experience emotional distress post-donation may find it reflected in a slower physical recovery, and vice versa. If a donor is experiencing extreme distress or low mood during any conversation with Anthony Nolan then this will be discussed with the medical officer immediately. If the donor is at risk of immediate harm the Anthony Nolan Safeguarding procedure (2) will be followed.
When speaking to donors for the day 2/3 follow up call, it is standard procedure to ask the donor about their emotional wellbeing. It may be appropriate at this point to bring this possible link between emotional and physical recovery to their attention, to encourage them to be aware of their recovery in a holistic sense and encourage them to reach out for support if needed.
If the donor notes feeling worse than usual emotionally, or notes any distress whether directly related to the donation process or in their own life, it may be appropriate to discuss the following with them:
- What are the things causing stress/distress now?
- Has the donation process itself impacted their emotional wellbeing, or brought up/amplified difficult emotions?
- What support do they have? (e.g. is there anyone in their family or friends, social/religious/work group that they feel comfortable talking to, or any activity that they find relaxing/a good distraction)
- If they don’t have any support in place; what kinds of things do they think may be helpful for them? (e.g. do they find talking helpful, or prefer to find other activities to distract them etc.)
If a donor feels worse emotionally after the donation, DFU will offer a second follow-up phone call a week after donation to check in on their wellbeing. If in this call a donor is still experiencing low mood or distress, then it should be discussed with the DFU Manager and the Medical team. It may be appropriate to offer the option of counselling sessions with Anthony Nolan’s counsellor, or the Medical team may advise the donor to see their GP for further support. This will be decided on a case-by-case basis.
DFU does not provide counselling or psychological support for the donor themselves but, following the training and guidance from regular clinical supervision sessions, offers a safe and non-judgmental space for the donor to talk through how they are feeling. Through these discussions DFU will gather the relevant information from the donor to share with the Medical Team and DFU Manager to determine next steps.
Peripheral Blood Stem Cell (PBSC) and Bone Marrow (BM) Recovery Graphs
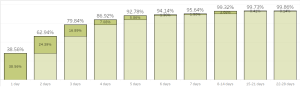
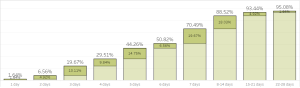
These graphs show the overall recovery times for PBSC and BM donors between 2020 and 2022.
95% of PBSC donor are fully recovered by day 7, and 99% by day 14. For BM donors, full recovery may take a little longer with 70% being fully recovered by day 7, 88% by day 14, and 95% by 1-month post-donation.
The 0.2% of PBSC donors, and 5% of BM donors who are not recovered by 1-month post-donation are followed up and managed by DFU and the Medical Team until the donor is fully recovered.
Graph A: Cumulative Duration to Full Recovery (PBSC) January 2020-Janurary 2022 from Anthony Nolan Donor Follow Up Tableau Dashboard (3)
Graph B: Cumulative duration to full recovery (Bone Marrow) January 2020-Janurary 2022 from Anthony Nolan Donor Follow Up Tableau Dashboard (4)
Guidance for Short Term Post-Donation Symptoms A-Z
Abdominal Swelling and Pain or Discomfort
PBSC Only
Anthony Nolan Recovery Data
No Anthony Nolan recovery data for infection at donation site is currently available. This section will be updated as and when this data is available.
Symptom Overview and Initial Conversation with Donor
The main concerns with pain and discomfort on the upper left side of the abdomen that develops during GCSF injections, or shortly after the donation (within 14 days), are issues relating to the spleen.
Many donors who receive GCSF will develop a slight enlargement of the spleen that settles after donation (5). However, in some rare cases there may be more serious complications.
If the donor is experiencing moderate to severe pain on the upper left side of the abdomen, and/or if they feel very unwell, weak, or faint; inform the Medical Team immediately and advise the donor to seek immediate medical attention.
If the swelling or discomfort is mild and/or not left sided, please ask:
- When did it start?
- How would they rate the pain/discomfort?
- Have they taken any painkillers? If yes, what painkillers did they take, and did it help?
- Where is the pain located? (e.g. all over the stomach/abdomen, or more in one area?)
- Have they recently had any injuries to their stomach or abdomen through impact/a fall, or have they recently done more strenuous exercise than usual?
- Any nausea, or feeling unusually full/bloated after eating small amounts?
- Any visible swelling across the stomach/abdomen?
- Any bruising, redness, or a rash?
Management of Symptoms
In most cases, enlarged spleen will return to normal within about 14 to 21 days. Flag the issue to the Medical Team in all cases, but if it is only mild swelling or discomfort of the upper abdomen, advise the donor that this should reduce over time. Advise them to avoid any situations where there is risk of impact to the area until it resolves (e.g. contact sports).
If the swelling continues for over 21 days, speak with Medical Team again, and if appropriate, they may refer the donor to their GP or to the Collection Centre for scans.
DFU to follow up with the donor until the swelling and pain or discomfort resolves.
Back Pain
Bone Marrow Only
Anthony Nolan Recovery Data
January 2020-2022: At day 2/3, 56% of donors note pain at donation site, 27% note stiffness, and 9% note muscular pain.
At day 7, 39% note pain at donation site, 37% note stiffness, and 24% note muscular pain.
At day 30 4% note pain at donation site, 4% note stiffness, and 5% note muscular pain (6).
Symptom Overview and Initial Conversation with Donor
Pain and discomfort around the donation site, along with stiffness and back ache, is very common for at least the first week post-bone marrow donation and may continue up to a month.
As advised in the Post-Donation Thank You Leaflet (DOC 1429), remind donors to avoid strenuous activities for 7-14 days, and encourage them to make a gradual return to their usual level of activity as they feel able to.
The donor may try the following to help alleviate the pain:
- Short walks may help with stiffness of the muscles and reduce pain
- Painkillers as needed. Donors may receive painkillers from the Collection Centre, but if not, they can take paracetamol or co-codamol (not to be used at the same time as both contain paracetamol), or they can use ibuprofen from 72 hours post-donation provided there are no complications such as bleeding from the donation site or extensive bruising, and the collection centre has not advised against using it (aim to use no longer than 14 days, and avoid this if they have any stomach ulcers or indigestion issues).
- If there is any mild swelling across the lower back, applying a cold compress or ice pack for 10 minutes at a time may help.
Management of Symptoms
If the back pain, stiffness, or discomfort is continuing at 4 weeks post-donation, or if the pain is severe, contact the Medical Team with a summary of the donor’s current symptoms.
Ask the donor:
- Any change, improvement, or worsening, of the back pain in the 4 weeks since donation?
- Location of the pain
- Is the pain constant, only after exercise, only at night etc.?
- Do they take any painkillers currently? If yes, what do they take and how often?
- Does light exercise or stretching help at all (if they have tried that)?
- How severe is the pain?
Send the responses to the Medical Team to discuss further. If required, and if agreed by the Medical Team and DFU manager, the donor may be referred for physiotherapy for 4-8 sessions to support their recovery. DFU will send the referral letter to a local physio once permission has been received from the donor to share their details.
In cases of severe pain, the Medical Team may refer the donor to the specialist, Professor Hart at Joint Recon (https://www.jointrecon.com). DFU will send the referral letter by encrypted email to his secretary, Elizabeth Hart ahartmedsec@ccf.org, requesting a review and MRI if needed.
In both referral cases, a SAR will be raised by DFU. The donor is seen as a private patient and the SAR will be used to track their recovery and incurred costs. DFU will follow up with the donor until they are fully recovered.
Bruising at Donation Site
PBSC
Anthony Nolan Recovery Data
January 2020-2022: 35% of donors reported bruising at day 2/3, 5% at day 7, and 1% by day 30 (7).
Symptom Overview and Initial Conversation with Donor
Some bruising around the donation site is quite common in PBSC donors, especially if it took multiple attempts to place the needle. As advised in the Post-Donation Thank You Leaflet (DOC 1429), donors may also notice that they bruise more easily for a few days post-donation due to low platelet levels.
Ask the donor to send a photo of the bruised area if they describe the bruising as moderate-severe, if they are concerned about the bruising, or if they also note any of the following symptoms:
- Swelling, redness, or tenderness around the donation site (See also #Infection at Donation Site )
- Difficulty moving the affected arm, or pain when extending the arm
- Change in sensation to the arm/hands (e.g. pins and needles, or numbness)
- Arms or hands are paler than usual
- Dizziness, shortness of breath, or chest pain
Also ask if they take any prescription or over-the-counter medications. This is because some medications may increase the likelihood of bruising, which may be useful for the Medical Team to take into account.
Management of Symptoms
If the donor does not have any of the symptoms noted in the above section, and the bruising is mild; advise rest, elevation of the bruised area where possible, and ask them to get in touch if the bruise continues to spread or if any of the symptoms of concern mentioned above develop.
If the donor does have any of the symptoms noted in the above section, and/or the bruising is more significant, ask them to send a photo of the affected area. Send the photo along with a summary of the symptoms to the Medical Team for advice. They may advise that the donor is seen for a review, and can provide a referral letter to facilitate this. DFU will work with the donor to arrange a review at their GP, at the Collection Centre, or if more urgent action is required, at A&E.
DFU will follow up with the donor to ensure the bruising and any pain resolves.
BM
Anthony Nolan Recovery Data
January 2020-2022: 16% of donors noted bruising at day 2/3, 19% at day 7, and 2% at day 30 (6).
Symptom Overview and Initial Conversation with Donor Some bone marrow donors notice bruising at the donation site within a couple of days, and some may report bruising later once their dressing is removed and they can see the donation site.
If the donor reports bruising, ask them to send a photo of the affected area. Also check for any of the following symptoms of concern:
- Noticeable swelling or tenderness around donation site (See also #Infection at Donation Site )
- Bleeding on the dressing
- Moderate to severe pain (e.g. affecting their daily activity)
- Pain going down the legs
- Change in sensation to the legs (e.g. pins and needles, numbness etc.)
- Dizziness, shortness of breath, chest pain
Management of Symptoms
Ask the donor to send a photo of the affected area if they are able to take one. Send the photo along with a summary of their symptoms, and the date and Collection Centre at which the donation took place, to the Medical Team who can advise further.
If necessary, they may provide a referral letter for the donor to be reviewed at their GP or at the Collection Centre as appropriate depending on the location of the donor.
DFU is responsible for contacting the Collection Centre to arrange referral if necessary. If there are any immediate or urgent concerns, the Medical Team may advise that the donor is reviewed at A&E.
DFU will follow up with the donor to ensure the bruising and any pain resolves.
Headache
PBSC Only
Anthony Nolan Recovery Data
January 2020-2022: 10% of donors noted “other pain (headache/sore throat) at day 2/3, 3% at day 7, and none at day 30 (7).
Symptom Overview and Initial Conversation with Donor
Almost half of donors experience some form of headaches whilst having the course of GCSF injections prior to donation (5). However as noted in the statistics above, most headaches will settle shortly after stopping G-CSF, with 10% still experiencing headaches at day 2 post-donation (5).
If a donor already suffers from migraines, the donation process may also trigger it. Donors can take their usual medications for it, and ibuprofen or other NSAIDs are safe 2-3 days post-donation.
If the headache is very severe and the donor has any problems with vision (and this is not part of their usual migraine symptoms), please ask them to seek urgent medical help and inform the Medical Team. Otherwise, please ask:
- When did the headaches start?
- Where is the pain located (i.e. one side of their head, front or back or head)?
- How would they rate the pain? (mild, moderate, severe, or a scale of 1-10)
- Have they ever had migraines?
- What painkillers have they tried so far, if any?
- Any nausea, vomiting, or high temperature alongside the headaches?
Management of Symptoms
Inform the Medical Team of the donor’s responses to the above questions for further advice. They may advise that the donor is seen by their GP or at the Collection Centre for review, and can provide a referral letter for this. DFU will work with the donor to arrange this referral if needed.
DFU will follow up with the donor until the headaches resolve.
Infection at Donation Site
PBSC
Anthony Nolan Recovery Data
No Anthony Nolan recovery data for infection at donation site is currently available. This section will be updated as and when this data is available.
Symptom Overview and Initial Conversation with Donor
Signs of an infection at the donation site include:
- redness and swelling
- redness that tracks up the arm
- skin that feels warm to touch
- pain at donation site
- fever, and feeling generally unwell.
See also #Bruising at Donation Site
The following symptoms may indicate that there is a possibility of tracking cellulitis, a potentially serious infection in the deeper layers of skin, which would require immediate care. Inform the Medical Team immediately and advise the donor to seek urgent medical care if they are experiencing the following symptoms:
- Feeling generally unwell
- High fever
- Red, inflamed skin which is warm to touch
- Painful line on the skin which usually follows the route of a blood vessel from the donation/injection site.
Management of Symptoms
Ask the donor to send a photo of the affected area, and inform the Medical Team in all cases if there is a concern of infection. The Medical team may refer the donor to their GP or back to the Collection Centre for a review and antibiotics, or to A&E if more urgent care is needed.
If the donor develops an infection at the donation site within 7 days of donation, discuss with the Medical Team about raising this as a SAR and informing the Transplant Centre as this may also affect the recipient. DFU will follow up with the donor until they are recovered.
BM
Anthony Nolan Recovery Data
No Anthony Nolan recovery data for infection at donation site is currently available. This section will be updated as and when this data is available
Symptom Overview and Initial Conversation with Donor
Signs of post-donation infection include:
- Redness and swelling,
- Skin feeling warmer than normal around the donation site
- High temperature
- Feeling generally unwell
- Pain at the donation site.
Management of Symptoms
Ask the donor to send a photo of the affected area, and check for the above symptoms, but do inform the Medical Team in all cases if there is a concern of infection.
If there is concern about a local infection, the Medical Team may refer the donor back to the Collection Centre or to their GP for a review and antibiotics.
If the donor is generally very unwell, advise them to seek immediate medical attention at A&E, and inform the Medical Team who may advise that the Collection Centre should check the BM cultures.
If the donor develops an infection within 7 days of donation discuss with the Medical Team about informing the Transplant Centre as this may also affect the recipient.
DFU will follow up with the donor until they are recovered
Infections (Other), and Viruses
Anthony Nolan Recovery Data
No Anthony Nolan recovery data for infections and viruses is currently available. This section will be updated as and when this data is available
Symptom Overview and Initial Conversation with Donor
Donors may develop infections or catch viruses post-donation that are not directly linked to the donation itself. For example:
- Conjunctivitis
- Tonsilitis
- Sinus infection
- Flu
- Coughs
- Colds.
Symptoms that may indicate a general infection include:
- Fever
- Chills and sweats
- Coughs
- Congestions
- Muscle aches (such as a stiff neck)
- Headaches
- Fatigue
Some of these symptoms are also quite common post-donation symptoms, so it is important to speak with the Medical Team if there is any concern that the donor may have an infection shortly post-donation.
Before speaking with the Medical Team, gather the following information from the donor:
- When did the infection start, or when did they first notice the symptoms?
- What are their current symptoms?
- Have they seen their GP? And if so, what advice or prescription have they been given?
- If antibiotics were given; what kind, and how many days is the course for?
- Have they taken a COVID test?
Management of Symptoms
In all cases of a donor reporting an infection or virus within 7 days of donation, or reporting that they have started medication such as antibiotics; report it to the Medical Team who can advise if any action is needed.
Any cases of infections reported within 1 week of donation must be reported to the Transplant Centre straight away. Any infections reported over 1 week post donation, but within 1 month will be discussed with the Medical Team who will decide if it is necessary to report to the Transplant Centre or not. Certain infection such as Hepatitis or HIV must be flagged to the Medical Team even if reported over 1 month post donation. If in doubt, discuss with the Medical Team.
Muscle Cramps
Anthony Nolan Recovery Data
No Anthony Nolan recovery data for muscle cramps is currently available. This section will be updated as and when this data is available
Symptom Overview and Initial Conversation with Donor
Muscle cramps can be caused by low electrolytes (chemicals and minerals in the body that support normal body function)or changes to levels of electrolytes such as calcium and magnesium (8). Muscle cramps usually settle within a few days to 1 week post donation.
Leg cramps specifically may also be linked to Restless Leg Syndrome which has been noted in some donors post-donation. See #Restless Legs for more details.
It is important to make sure that the donor does not have any other symptoms associated with low calcium, such as:
- Tingling in arms and legs
- Tingling around the mouth
- Leg cramps getting gradually worse
Management of Symptoms
If the donor is experiencing any of the above symptoms; inform the Medical Team who may refer the donor for blood tests to check their calcium levels, and may advise the donor to start taking supplements straight away whilst waiting for the blood tests. DFU will liaise with the donor and either their GP or a private GP clinic to arrange the appointment if needed.
DFU to follow up with the donor until the cramps have resolved and the donor is fully recovered.
Nausea, Vomiting, and Diarrhoea
PBSC Only
Anthony Nolan Recovery Data
January 2020-2022: 3% of donors noted nausea/vomiting at day 2/3, 2% at day 7, and none at day 30 (7).
Symptom Overview and Initial Conversation with Donor
Nausea, vomiting, and diarrhoea are not as common as other symptoms, but GCSF is known to cause various stomach upsets in some donors (5). This usually settles shortly after stopping GCSF injections but do contact the Medical Team if there is any concern about the donor’s wellbeing.
Please ask the following questions to gather as much information as possible for the Medical Team:
- What symptoms do they currently have?
- When did the symptoms first start?
- Has it improved at all since stopping the GCSF injections?
- Is the nausea/vomiting/diarrhoea there all the time or does it come and go? If coming and going, is there any pattern (e.g. worse after eating/ worse in the mornings)?
- Are they managing to eat any food/ Are they eating similar amounts as before?
- Are they managing to keep drinking water or other liquids?
- Any weakness, dizziness, or fainting? (See also #Abdominal Swelling and Pain or Discomfort )
- Have they taken any medications for nausea?
- Any stomach pain/cramps? If yes, is the pain more noticeable on the left side? (See also #Abdominal Swelling and Pain or Discomfort )
The Medical Team should be informed in all cases of left sided abdominal pain, or if donor is unable to keep drinking water or feels week, dizzy or faint.
Management of Symptoms
Usually, nausea will settle within 48 hours of stopping GCSF injections. The following things might be helpful and should be encouraged:
- Continuing to drink plenty of water
- Eating small amounts of food frequently, rather than large meals
- Herbal teas like ginger or peppermint tea
If the nausea, vomiting, or diarrhoea is ongoing beyond 2 days post-donation, or if the donor is very unwell; inform the Medical Team who can advise further. There is also a medication available over the counter for nausea called Buccastem M, containing an ingredient which can reduce nausea. The Medical Team can advise the donor about this if they feel it is an appropriate treatment for them. If the symptoms are determined to be related to an infection, then the transplant centre must also be informed. See #Infections (Other), and Viruses DFU will follow up with the donor until the nausea, vomiting, or diarrhoea is resolved.
Pain and/or Tingling at the Donation Site
PBSC only
Anthony Nolan Recovery Data
January 2020-2022: 11% noted pain at donation site at day 2/3, 3% at day 7, and none at day 30 (7).
Symptom Overview and Initial Conversation with Donor
If the donor notes any pain at the donation site, ask for further information:
- How would they describe the sensation? (e.g. dull ache, sharp pain, ‘shooting’, ‘tingling’, ‘pins and needles’ etc.)
- How severe is the pain?
If it is described as ‘shooting’, ‘tingling’, or ‘pins and needles’ and developed either straight away when the needle was inserted, during the donation procedure, or shortly after donation, it may have been caused by the needle irritating a nerve. Check for any of the following symptoms:
- Swelling or tenderness around the donation site (See also #Infection at Donation Site)
- Difficulty flexing or extending the arm as normal,
- Significant pain when flexing or extending the arm
- Change in sensation to the arm/hands? (e.g. Numbness, unable to feel hot or cold)
- Unusually pale arms or hands
Management of Symptoms
If the pain is mild and the donor answered no to all the above symptoms, advise the donor to avoid strenuous activity for a few days, and that it may settle within 7 days. If the pain/discomfort lasts longer than 7 days, inform the Medical Team who can consider referring to the GP for support such as pain relief specific to nerve pain, physiotherapy, or other investigations such a scan if appropriate.
If the pain is more significant, and/or the donor answered yes to any of the symptoms above; inform the Medical Team for further advice. The donor may be referred to their GP, back to the Collection Centre, or to A&E for a review and scans of the affected area depending on the severity of the symptoms.
If further investigations are needed, DFU will arrange the referrals with donor’s agreement, and follow up until they are recovered.
Pain at G-CSF Injection Site
PBSC Only
Anthony Nolan Recovery Data
January 2020-2022: 1% of donors reported pain at injection site at day 2/3, and none at day 7 or day 30 (7).
Symptom Overview and Initial Conversation with Donor
Review this along with questions as in #Infection at Donation Site.
First ask the donor to describe the pain (e.g. sharp/dull pain, constant or only at certain times, does it radiate out to other areas etc.). Check the how long it has been since the donation and since the last G-CSF injection, and ask the donor if they have any of the following symptoms:
- Swelling or redness around the injection site
- Skin that is hot to touch around the injection site
- Significant bruising
- Lumps under the skin at the injection site
- Pain across the stomach
- Temperature, feeling generally unwell, or very tired
- Chest pain, shortness of breath, or dizziness
- Other visible changes around the injection site
Management of Symptoms
If the donor answers no to all the above, advise them to try painkillers like paracetamol, and consider using an ice pack, compress, or local anaesthetic sprays or creams to ease the discomfort while the injection site is healing.
If they answer yes to any of the above or if there is any concern about infection, inform the Medical Team and include as much detail about the current symptoms as possible.
The Medical Team may refer the donor back to the collection centre or to their GP for review if appropriate. DFU will liaise with the donor and the collection centre or GP to arrange this if necessary. If the donor is feeling generally very unwell the Medical Team may advise them to seek more immediate medical attention.
DFU will follow up with the donor until the pain resolves.
Rash
Anthony Nolan Recovery Data
January 2020-2022: 1% of donors reported a rash at day 7 and day 30 post-donation, and none at day 2/3 (9).
Symptom Overview and Initial Conversation with Donor
Donors may develop a rash in reaction to new medications or new materials they encounter during the donation process (e.g. the hospital’s clothes, alcohol swabs etc.). Usually, this settles shortly after the cause of the rash is removed. However, it is important to confirm if it is just a rash, or if it is a sign of infection.
First check if the donor has had any facial swelling or difficulty breathing. If yes, advise them to seek urgent medical help and inform the Medical Team immediately. This situation will be extremely rare.
Otherwise, please ask the following questions to gather more information for the Medical Team:
- When did they first notice the rash?
- Is it getting any worse/ staying the same/ getting any better?
- Is it itchy?
- Has anyone else in their household developed a similar rash?
- Have they had similar rash before? If so, when did it happen and what caused it?
- Have they recently taken any new medications or supplements?
- Have they been feeling feverish? Had a temperature? Had any other viral symptoms?
- Do they have any allergies?
Management of Symptoms
In all cases of a reported rash, ask the donor to send a picture of the affected area, and forward this, along with the responses to the above questions and anything else noted by the donor, to the Medical Team for further advice.
DFU to follow up until the rash has resolved.
Restless Legs
Anthony Nolan Recovery Data
No Anthony Nolan recovery data for restless legs is currently available. This section will be updated as and when this data is available
Symptom Overview and Initial Conversation with Donor
There have been some cases noted by Anthony Nolan, and by DKMS, of donors developing restless leg syndrome post-donation. Symptoms can include:
- An urge to move the legs, usually worse in the evening or at night
- Crawling sensation in the legs
- Involuntary movements
With any leg symptoms, it is also important to rule out deep vein thrombosis (DVT).
Ask if the donor has any of the following symptoms:
- Any leg swelling? If yes, is it in both legs or just one?
- Any leg pain? If yes, where is the pain located?
- Any visible redness of the legs?
- Any shortness of breath?
If any of the above are present, contact the Medical Team urgently. The donor may need to attend A&E to be reviewed for DVT.
If no to the above symptoms, restless legs should resolve over time and without intervention. However, the following may also help to reduce the symptoms:
- Good sleeping routine (regular sleep schedule, enough time to ‘wind down’ before bed, no alcohol or caffeine before sleep)
- Regular but gentle exercise during the daytime
- Warm compresses or baths
- Distraction/relaxation techniques
- Quitting smoking if they currently smoke
Management of Symptoms
Restless leg syndrome can be made worse by, or caused by, iron deficiency anaemia, electrolyte imbalance (calcium and magnesium), and low vitamin D or B12 levels. Therefore, the Medical Team may refer the donor to their GP for blood tests to check these.
If the symptoms are causing distress and do not seem to be improving, the Medical Team may refer the donor to their GP with a request for consideration of appropriate medication or other treatment.
DFU will follow up with the donor until the symptoms resolve.
Tiredness
PBSC
Anthony Nolan Recovery Data
January 2020-2022:58% of donors reported tiredness at day 2/3, 6% were still reporting tiredness at day 7, and 3% by day 30 (7).
Symptom Overview and Initial Conversation with Donor
We know that female donors, older donors, and donors who donated over 2 days may feel tired for longer and take longer overall to fully recover (10), (11). As noted in the Post-Donation Thank You Leaflet (DOC 1429), advise donors to rest and avoid strenuous activities for 48 hours, and keep well hydrated.
Contact the Medical Team for further advice if the donor notes any of the following symptoms alongside the tiredness:
- breathlessness with even gentle exercise (e.g. daily activities, walking etc.)
- chest pain
- dizziness
- fainting
Management of Symptoms
If the donor does not note any of the above symptoms; advise them to rest, keep well hydrated, and get in touch if they do start to have any of the symptoms listed above.
If the tiredness continues over 7 days post-donation, contact the Medical Team to discuss. The Medical Team may refer the donor to their GP for repeat blood tests if appropriate. DFU will liaise with the donor to arrange the appointment.
DFU will send any referral letters from the Medical Team to the donor and their GP, and will continue to follow up until the donor is fully recovered.
BM
Anthony Nolan Recovery Data
January 2020-2022:70% of donors reported tiredness at day 2/3, 39% were still experiencing tiredness at day 7, and 7% at day 30 (6).
Symptom Overview and Initial Conversation with Donor
As noted in the Post-Donation Thank You Leaflet (DOC 1429) donors may experience a period of severe tiredness for 5-6 days post-donation. They may also have some difficulty sleeping, and light-headedness when waking up in the morning which may add to the overall sense of tiredness.
Advise donors to take it easy especially in the morning, and to have small, regular meals, and early nights to help return to a regular sleeping pattern. Strenuous activity should be avoided for 7-10 days post-donation to allow time for the body to recover from the donation procedure.
Check if the donor is experiencing any of the following symptoms alongside tiredness:
- breathlessness with exercise
- chest pain
- dizziness
- fainting
- severe tiredness where they are unable to do some normal daily activities (e.g. walking from room to room)
Management of Symptoms
If yes to any of the above symptoms, contact the Medical Team for further advice. If no to the above symptoms, but the tiredness continues beyond 14 days post-donation, contact the Medical Team for further advice. The donor may be advised to book a GP appointment for follow up blood tests if tiredness is ongoing over 2 weeks post-donation. This may help to identify the cause of the ongoing tiredness (such as low iron levels for which the donor’s GP may prescribe iron supplements).
DFU will continue to follow up with the donor until they are fully recovered.
References
- Burlton, Catherine et al. "Young Donor Project Exec Summary Version 1". 2021. Anthony Nolan accessed 19 December 2022 https://www.anthonynolan.org/sites/default/files/2021-05/2526OP_Young%20Donor%20Project%20Exec%20Summary.pdf
- Lovell, Terence. "Anthony Nolan Safeguarding Policy and Procedures V6". 2020. Anthony Nolan accessed 7 January 2023 https://matchbook.anthonynolan.org/sorce/beacon/dmd/1197/view/Anthony%2BNolan%2B-%2BSafeguarding%2BPolicy%2B-%2BRevised%2BJuly%2B2020%2BReviewed%2BJan%2B2021.pdf
- Graph A: Cumulative Duration to Full Recovery (PBSC), Tableau, accessed June 7, 2023, https://eu-west-1a.online.tableau.com/#/site/anthonynolan/views/Donorrecoverypost-donation/Recoverytimes?:iid=1 Results filtered by: Donation Type: PBSC, Date of Response Received range set to: January 2020 to January 2022
- Graph B: Cumulative duration to full recovery (Bone Marrow), Tableau, accessed June 7, 2023, https://eu-west-1a.online.tableau.com/#/site/anthonynolan/views/Donorrecoverypost-donation/Recoverytimes?:iid=1 Results filtered by: Donation Type: BM, Date of Response Received range set to: January 2020 to January 2022
- Hölig, Kristina. "G-CSF In Healthy Allogeneic Stem Cell Donors". Transfusion Medicine And Hemotherapy, vol 40, no. 4, 2013, pp. 225-235. S. Karger AG, https://doi.org/10.1159/000354196.
- Frequencies Symptoms Reported by Donors Post-Donation, Tableau, accessed August 15, 2022, https://eu-west-1a.online.tableau.com/#/site/anthonynolan/views/Donorrecoverypost-donation/Symptomfrequencies?:iid=1. Results filtered by: Donation Type: BM, Time Point Post Donation: Day 2/3, Day 7, Day 30, Date of Response Received range set to: January 2020 to January 2022
- Frequencies Symptoms Reported by Donors Post-Donation, Tableau, accessed August 15, 2022, https://eu-west-1a.online.tableau.com/#/site/anthonynolan/views/Donorrecoverypost-donation/Symptomfrequencies?:iid=1. Results filtered by: Donation Type: PBSC, Time Point Post Donation: Day 2/3, Day 7, Day 30, Date of Response Received range set to: January 2020 to January 2022
- Stroncek, David F., and Lee England. “Protecting the Health and Safety of Cell and Tissue Donors.” ISBT Science Series, vol. 10, S1, 12015, pp. 108–114., doi:10.1111/voxs.12150.
- Frequencies Symptoms Reported by Donors Post-Donation, Tableau, accessed August 15, 2022, https://eu-west-1a.online.tableau.com/#/site/anthonynolan/views/Donorrecoverypost-donation/Symptomfrequencies?:iid=1. Results filtered by: Donation Type: All, Time Point Post Donation: Day 2/3, Day 7, Day 30, Date of Response Received range set to: January 2020 to January 2022
- Pulsipher, Michael A et al. “Acute toxicities of unrelated bone marrow versus peripheral blood stem cell donation: results of a prospective trial from the National Marrow Donor Program.” Blood vol. 121, no1, 2013, pp. 197-206. doi:10.1182/blood-2012-03-417667
- Shaw, Bronwen E et al. “Analysis of the Effect of Race, Socioeconomic Status, and Center Size on Unrelated National Marrow Donor Program Donor Outcomes: Donor Toxicities Are More Common at Low-Volume Bone Marrow Collection Centers.” Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation vol. 21, no.10, 2015, pp.1830-1838. doi:10.1016/j.bbmt.2015.06.013
Version
Version 2
Date of Last Update
12th June 2023